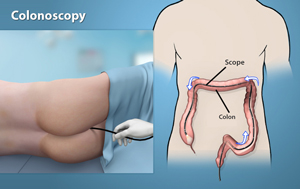
Colonoscopy
Colonoscopy is an endoscopic procedure used to view the large intestine (colon and rectum) using an instrument called colonoscope (a flexible tube with a small camera and lens attached at one end). The procedure can detect inflamed tissue, ulcers, and abnormal growths. It is used to diagnose early signs of colorectal cancer, bowel disorders, abdominal pain, muscle spasms, inflamed tissue, ulcers, anal bleeding, and non-dietary weight loss.
Colonoscopy is performed under general anesthesia. The colonoscope is inserted into the rectum which gently moves up through the colon until it reaches the caecum (junction of small and large intestine). Colonoscopy provides an instant diagnosis of many conditions of the colon and is more sensitive than X-rays.
The colonoscope is then withdrawn very slowly as the camera shows pictures of the colon and rectum on a large screen. Polyps or growths can also be removed by colonoscopy which can be sent later for detection of cancer.
Instructions for colonoscopy
Your physician may provide you written instructions and also will communicate on how to get prepared for the colonoscopy procedure. The process is called bowel preparation.
Gastrointestinal (GI) tract should be devoid of solid food; a strict liquid diet should be followed for 1 to 3 days before the procedure. Patients should not drink beverages containing red or purple dye. Liquids that can be taken before surgery include fruit juices, plain coffee, tea and water.
Certain medications such as aspirin, ibuprofen, naproxen or other blood thinning medications, iron- containing preparations should be stopped before the test. Iron medications produce a dark black stool, and this makes the view inside the bowel less clear.
A laxative or an enema may be required the night before colonoscopy. Laxatives loosen the stools and increase bowel movement. Laxatives are usually swallowed in pill form or as a powder dissolved in water.
Driving is not permitted for 12 hours after colonoscopy.


